While the intersection of fat liberation and parenting can be an amazing counter-cultural, anti-oppression practice, it can also feel like a lonely place.
But you're not alone and you deserve community. That's why I'm creating a Fat Parent Group. The Group will be an opportunity to gather with other fat parents who *get* it; receive and lend support; and process the joys & challenges of raising resilient children. The group will be facilitated by me, Laurie Ganberg, LICSW (fat therapist and parent), but it's not therapy. It's a chance to gather with other fat parents who value raising kids to trust their bodies, free from diet-culture and anti-fat bias. And you can join from anywhere! Meeting on the second Wednesday of the month in 2023: August 9, September 13, October 11, November 8, December 13 @ 4:00-5:15pm (PST) Logistics
Dear Perinatal Mental Health Therapists,
Please take 3 minutes to answer a few questions. The survey is anonymous, unless you choose to share your email address to learn about upcoming trainings. You are also welcome to follow me on instagram (@laurieganberglicsw) if you'd rather learn about upcoming trainings there. And feel free to email me at [email protected] with any questions! thanks, Laurie
Intrusive thoughts continue to be one of the most challenging symptoms I see people experience in pregnancy, postpartum, and beyond. It's so easy to misunderstand them, few people talk about them, and these sticky thoughts often center on the very things that most upset us.
I'm going to share more information for partners/family members and for therapists in future posts, but to start with, here are five quick facts that might help you understand what's going on if you're experiencing intrusive thoughts.
If you're experiencing significant distress or worry about your intrusive thoughts, you can feel better. And as scary as it seems, talking to someone who understands perinatal intrusive thoughts is a good place to start. If you're not sure who that is in your life, contact the Postpartum Support International HelpLine at 1-800-944-4773.
If you feel like you're in crisis, you can call 988 to be connected to your local crisis team. There's also the 24/7, confidential Maternal Mental Health Hotline: 1-833-943-5746. Book Resources:
I participate in an Affiliate program with Bookshop.org, an online bookstore "with a mission to financially support local, independent bookstores." A purchase from my link will pay me a small commission, and gives a matching percentage to independent bookstores. You can view my Bookshop "shop" here: https://bookshop.org/shop/laurieganberglicsw. These recommendations do not constitute medical advice or a therapeutic relationship.

"Being with" is a concept that shows up a lot when you're a therapist, supervisor, and parent; and it's illustrated beautifully in the children's book The Rabbit Listened by Cori Doerrfeld.
The urge to fix — to provide a solution, to solve a problem, to make your kiddo happy again — is powerful and comes from a place of wanting to help. Yet, this instinct can be the opposite of helpful. You've heard the folks who say, "hey, just relax!" in response to someone's worries, right? It comes across as invalidating, condescending, and definitely unhelpful. When we're able to be with someone in their experience, we can be curious, we can better understand, and ultimately, we can probably be more helpful. In Doerrfeld's book, the rabbit comes along to provide a compassionate presence and and a listening ear; eventually, the child is able to share their story, their emotions, and figure out what to do next. In therapy and supervision, I aim to be a compassionate, nonjudgmental presence and I try to notice those urges to fix when they come up. In doing so, I hope I'm also modeling and supporting my clients in learning how to be with their own experiences and emotions. (The opposite of this is mindless social media scrolling, Netflix binges, etc — a fine distraction some of the time, but not very useful as a long-term strategy.) In the realm of parenting, it can feel even harder. Being with your child in their hurt, sadness, anger, shame, or fear can feel excruciating. When we can do that, we demonstrate that these emotions are tolerable and not something to be feared, avoided, or pushed away. And, when we let go of the responsibility of making our children happy (something we can't really do anyway) there's a sense of relief. All we have to do is be there and listen.
I participate in Bookshop.org's affiliate program. You can see more recommendations at https://bookshop.org/shop/laurieganberglicsw. If you end up buying a book through one of my links, I earn a small commission and they donate the same amount to independent bookstores. Many, if not all, of these books can also be accessed through our amazing public library system, often as physical books, ebooks, or audiobooks!
 Photo by Jerry Wang on Unsplash Photo by Jerry Wang on Unsplash
I find myself often recommending the same few books to clients, colleagues and friends so I thought I'd start sharing them here. And, as a former small, independent bookstore employee in college, I'm excited to participate in Bookshop.org's affiliate program. If you end up buying a book through one of my links, I earn a small commission and they donate the same amount to independent bookstores. Many, if not all, of these books can also be accessed through our amazing public library system, often as physical books, ebooks, or audiobooks!
One of my favorites...
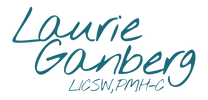
Coping During COVID CrisisLower expectations. Rest when you can. Remember this period of physical isolation will not last forever. If anxiety, panic, or adrenaline is spiking, try one — or aim for a bingo — of these grounding and distress tolerance skills to calm your activated nervous system. If you need more support, text HOME to 741741 for the Crisis Text Line. I’m offering telemental health aka online therapy along with many other therapists during this “Stay at Home” social distancing time. You can read more about my teletherapy services here. You can contact Postpartum Support International to find a therapist in your area and therapists doing online therapy.
I wrote a piece about ambivalence in motherhood for Perinatal Support Washington's newsletter for professionals and then was asked by PEPS to adapt it for families. You can read it also in the PEPS newsletter here: https://blog.peps.org/2018/11/07/i-love-my-baby-but-i-miss-my-old-life/ I love my baby, but I miss my old life.“I love my baby but I feel trapped.”
“Maybe having a baby was a mistake.” “Every part of my life has changed. I miss my old life.” I often hear these statements hesitantly shared by women experiencing ambivalence and regret after a new baby—along with, “I can’t talk about this in the new moms group.” But it is possible to find ways to hold these experiences without judgment, so that you can share the thoughts that have been swirling around in fear, guilt, and hopelessness. These feelings occur to many women – and their partners – after having a baby. You are not alone. In my work with new mothers we’re making space for feelings of ambivalence, regret, grief and loss that might come along with a new baby. “How has motherhood been, compared to what you thought it would be like?” Reflecting on what your expectations were and from where they came can help. Messages from partners, grandparents, Instagram, even strangers at the grocery store can morph into one loud proclamation: “You’re supposed to love this baby and this experience of parenting unconditionally.” In reality, we know that’s not always the case and we can work on tolerating a range of feelings and experiences of motherhood. You can love your baby and not love the baby stage at the same time. “Not everyone feels an overwhelming burst of love for their baby at the birth. Some do, but for others, it comes a few weeks or even months later. Not feeling it now doesn’t mean you won’t ever feel it. How has it been for you?” When you’re not feeling connected to baby, it can feel like it won’t ever get better and there must be something wrong with you. Yet not everyone has a made-for-TV moment with baby right after the birth. A scary birth experience, past trauma, or NICU stay can be a factor; sometimes, the love just takes longer to build. I’ve seen it happen. Connecting with a newborns can also be challenging. They’re not great conversationalists. They won’t tell you you’re doing a good job. And the job never really seems to be complete. We start seeing more social smiles and sustained eye contact at about 6-8 weeks. Around 3 months they’re starting to try to grab for things. Understanding the rough guidelines for infant development can help you know what’s coming and put some of the challenges in context. “What are you doing with your baby?” Take a moment to acknowledge all that you are doing with and for your children. Sometimes parents feel pressure to be doing or teaching more. Those emails you might receive saying, “at this age, your baby should be…” can reinforce this. But what babies need most is for you to simply “be with” them, comfort them, feed them. All these moments can feel insignificant, especially if you feel like you are going through the motions, but these actions are the foundation of a secure attachment. So recognize that even if you’re not feeling like you’re doing enough, you can be still be meeting baby’s needs and building a connection. Ambivalence can emerge no matter how challenging or how easy the tasks of parenting feel. But there are also larger stressors that can make things more difficult, such as
Coping with and managing feelings of ambivalence and regret is challenging, but my hope is that by making space for a range of experiences of motherhood, including ambivalence and regret, we can lessen the feelings of shame, fear, and despair. What can you do?
 “How did they let me leave the hospital with this brand-new baby? How will I keep him alive?” This is a common refrain voiced by new parents in the first few days after their baby is born. After all, there’s a steep learning curve to feeding and diapering a newborn, getting enough sleep and adjusting to a new normal. Unfortunately, a large number of new parents (mothers and fathers) also experience intense anxiety that something bad will happen to their baby. We just don’t talk about it. Disturbing thoughts don’t mean you’re crazy. For some, this distressing fear is experienced as unwanted images or thoughts. They’re scary, uncontrollable and feel like they’re playing on a loop in the parent’s mind. The thoughts are disturbing and can include someone — maybe even the parents themselves -- harming the baby. Parents I see at the Swedish Center for Perinatal Bonding & Support sometimes share these scary thoughts with me. Their first questions are, “I would never do anything to hurt my baby! Why am I thinking these things?” and “Am I going crazy?” In fact, these thoughts are symptoms of anxiety, depression or obsessive compulsive disorder, which can occur during and after pregnancy. By themselves, these thoughts don’t mean a parent will do anything to harm a baby. Maternity-related anxiety is common and treatable Talking about intrusive thoughts, anxiety and depression is hard. Women feel ashamed and worried that if they disclose their symptoms, someone’s going to take their baby away or think they aren’t good mothers. While postpartum depression has received media attention, ongoing silence around intrusive thoughts contributes to ongoing stigma and feelings of isolation for new parents. Nearly 1 in 5 women and 1 in 10 men experience depression or anxiety after the birth of a baby. For many of the women, their symptoms started in pregnancy. Anyone can experience these symptoms, but factors that increase a woman’s risk include:
This group will be a chance to gather with and get to know a small group of other pregnant women while learning -- and practicing -- a number of strategies that can help you create more peace in your pregnancy, birth, and motherhood. You can read more about the group here.
 I thought I'd take a moment to answer a few common questions I encounter when speaking with prospective clients. Have a question that isn't answered here? Comment below or you can always feel free to contact me. Whether it's due to fear about divulging the thoughts that keep you up at night, hesitation about "starting over" with a new provider, or just the quagmire of finding a therapist who takes your insurance and has openings, reaching out to find a new therapist can be challenging and anxiety-provoking. Wondering about these additional questions is unnecessary. Q: "I see from your website that you specialize in working with pregnant and postpartum women. Can I still see you for therapy if I'm not pregnant/postpartum/a woman?" A: Yes! While I do have a specialty in perinatal mental health and women's reproductive health, I also see adults and adolescents who are neither pregnant nor parenting. And I welcome transgender individuals and men to my practice. I enjoy working with a wide range of people; each brings a multitude of identities and struggles to therapy. The best way to determine if I might be a good fit for you is to schedule a phone consultation. Q: "I have Tufts Health Insurance. Do you accept that?" A: I accept "Tufts Health Plan - Public Plans." These are typically the Tufts Health Plan products that you would have if you have MassHealth or purchased your insurance through the Health Connector. You might have had "Network Health" previously. I do not accept Tufts Health commercial plans at this time. Typically, if you have Tufts insurance through your or your partner's employer, that is a commercial plan. You can always call the Member Services phone number on your health insurance ID card and ask them if I am an in-network provider for outpatient psychotherapy services for your plan. My NPI number is 1639208234. It's always a good idea to confirm that a provider is covered by your individual health insurance. Q: "Can I bring my baby with me to therapy?" A: Probably, yes. I am well aware of how hard it is to find time without the baby to go to appointments. I attempt to make therapy as easy as possible for you to access and if bringing your baby is necessary, they are welcome. I have an activity mat and some toys (though they often also like playing with an empty paper cup!), and the office is big enough for your stroller or carseat. I also have a chair that's comfortable for feeding your baby if necessary. The easiest babies to accommodate in therapy are non-mobile ones. A word of caution that some parents find it challenging to speak openly with their babies in the room - even very young infants. And if it works for you and you'd prefer to leave the baby at home, that's obviously ok, too. Q: Can you help me find a prescriber or complementary practitioner? A: There are many modalities that can alleviate depression, anxiety, and other emotional complications. In my previous clinical work, I helped families create teams of providers all working together to support a child and their family. I've kept that perspective in this work. If medication might be helpful, I can help you talk with your existing medical providers or refer you to a psychopharmacologist. I also regularly refer to acupuncturists, chiropractors, physical therapists, massage therapists, doulas, and lactation professionals.
Asking for help is a sign of strength and finding the right therapist shouldn't be a barrier to feeling better.
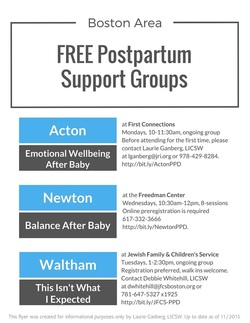 Latest update of the flyer of FREE postpartum support groups that focus on postpartum emotional complications like postpartum depression, mood, and anxiety disorders. This is a great resource for birth, postpartum, and lactation professionals to share with clients while providing education about prevalence, risk factors and signs to look out for. Other postpartum groups can be found at the Postpartum Support International of Massachusetts website. The next session of my postpartum group will start in January 2016. Adjusting to Motherhood is a small, 6-week group for women experiencing adjustment challenges or emotional complications in the postpartum year or after adopting an infant. Learn more about Adjusting to Motherhood...
 I'll be collecting the donations at the East Branch of the Somerville Library to bring to the WIC office. I'll be collecting the donations at the East Branch of the Somerville Library to bring to the WIC office. Diapers are expensive. And yet, there are few resources to help families in poverty afford them -- WIC doesn't provide diapers, and "food stamps" or SNAP benefits won't cover diapers (or wipes!) either. One study found that 1 in 3 low-income families cannot afford enough diapers for their children. When you can't change your baby's diaper, you can't soothe your baby. Unsurprisingly, this leads to increased stress levels, depression and anxiety for parents. Three years ago, Kerstin Sinkevicius and Aimee Mills - two moms who met through the Somerville Moms yahoo group - started a diaper drive to collect diapers to donate to the WIC office that serves Somerville, Cambridge, Arlington, Watertown, Lexington, and Belmont. Last year, they collected 22,674 diapers which were distributed to over 200 families. This year, they hope to collect 30,000 during the drive, which is running from September 19 to October 4. There are drop off boxes around Somerville, Cambridge, Arlington, Watertown and Lexington, including one in my building upstairs at Acupuncture Together, and the one pictured above at the Somerville Library East Branch. There are also registry links set up through Amazon, Diapers.com, and Target to buy diapers and have them sent directly to WIC. Check out the Somerville Diaper Drive website for more information. This is an easy, tangible way to support families in this community. If you're able, please consider donating some diapers!
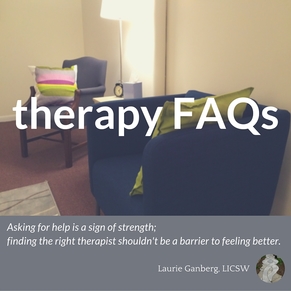
You've heard of PPD or postpartum depression. But what about perinatal emotional complications? Check out the infographic to learn 5 surprising facts about perinatal emotional complications. Sources are listed below.
Update: I've had some requests for hardcopies of this infographic, so I created a free PDF you can download.
[click infographic to enlarge]
Sources
Bornstein, D. (2014, October 16). Treating Depression Before It Becomes Postpartum. The New York Times. Retrieved from http://opinionator.blogs.nytimes.com/2014/10/16/treating-depression-before-it-becomes-postpartum/?_r=1
Dennis, C. L., & Chung‐Lee, L. (2006). Postpartum depression help‐seeking barriers and maternal treatment preferences: A qualitative systematic review. Birth, 33(4), 323-331. DOI: 10.1111/j.1523-536X.2006.00130.x. Foli, K. J. (2009). Postadoption depression: What nurses should know. AJN The American Journal of Nursing, 109(7), 11. DOI: 10.1097/01.NAJ.0000357144.17002.d3. Goodman, Janice H., and Lynda Tyer-Viola. Detection, treatment, and referral of perinatal depression and anxiety by obstetrical providers. Journal of Women's Health 19.3 (2010): 477-490. DOI:10.1089/jwh.2008.1352. Hamm, N. (2014, November 25). High Rates of Depression Among African-American Women, Low Rates of Treatment. Retrieved from http://www.huffingtonpost.com/nia-hamm/depression-african-american-women_b_5836320.html Hobfoll, S. E., Ritter, C., Lavin, J., Hulsizer, M. R., & Cameron, R. P. (1995). Depression prevalence and incidence among inner-city pregnant and postpartum women. Journal of Consulting and Clinical Psychology, 63(3), 445. http://dx.doi.org/10.1037/0022-006X.63.3.445 Howell, E. A., Mora, P. A., Horowitz, C. R., & Leventhal, H. (2005). Racial and Ethnic Differences in Factors Associated With Early Postpartum Depressive Symptoms. Obstetrics and Gynecology, 105(6), 1442–1450. DOI:10.1097/01.AOG.0000164050.34126.37. Huang, H. L., Peng, L., Zheng, S., & Wang, L. S. (2014). Observation on therapeutic effects of acupuncture plus psychological intervention for postpartum depression. Journal of Acupuncture and Tuina Science, 12(6), 358-361. DOI:10.1007/s11726-014-0805-7. Kim, P., & Swain, J. E. (2007). Sad Dads: Paternal Postpartum Depression.Psychiatry (Edgmont), 4(2), 35–47. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2922346/ Kozhimannil, K. B., Trinacty, C. M., Busch, A. B., Huskamp, H. A., & Adams, A. S. (2011). Racial and Ethnic Disparities in Postpartum Depression Care Among Low-Income Women. Psychiatric Services (Washington, D.C.), 62(6), 619–625. doi:10.1176/appi.ps.62.6.619. Nonacs, R. (2015, February 26). Treating Depression During Pregnancy Prevents Postpartum Depression. Retrieved from http://womensmentalhealth.org/posts/treating-depression-pregnancy-prevents-postpartum-depression/ Ross, L. E., Steele, L., Goldfinger, C., Strike, C. (2007). Perinatal depressive symptomatology among lesbian and bisexual women. Archives of Women's Mental Health. 10,(2), 53-59. DOI: 10.1007/s00737-007-0168-x. Smith, M. V., Kruse, A., Weir, A., & Goldblum, J. (2013). Diaper need and its impact on child health. Pediatrics, 132(2), 253-259. DOI: 10.1542/peds.2013-0597. Wisner, K. L., Sit, D. K., McShea, M. C., Rizzo, D. M., Zoretich, R. A., Hughes, C. L., ... & Hanusa, B. H. (2013). Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA Psychiatry, 70(5), 490-498. DOI: 10.1001/jamapsychiatry.2013.87. 
Two interesting news items related to postpartum depression popped up this past week. The first is news that researchers have identified a link between an oxytocin receptor blood marker in some women which increased their likelihood of experiencing postpartum depression. What does this mean? Well, if there were a blood test to give pregnant women to identify which ones were more likely to experience postpartum depression, we could proactively identify those women, doctors and families could put supports into place for the postpartum period ahead of time.
The second story is about a change in recommendations from the US Preventive Services Task Force about screening adults for depression. Now, if you're like me, you might be asking yourself what the US Preventive Services Task Force (USPSTF) is and what they do. Turns out, The Task Force is convened by Congress and reviews current clinical research to "improve the health of all Americans by making evidence-based recommendations about clinical preventive services such as screenings, counseling services, and preventive medications." This Task Force is now recommending that all adults be screened for depression because of its prevalence (1 in 10 all adults in the US will experience depression), and they specifically identified that all pregnant and postpartum women be screened. My reactions
It's great when postpartum depression gets media attention. It increases awareness of the huge number of families affected by emotional complications in pregnancy and postpartum . Screening and identifying those who are suffering is a critical first step.
However, there's an immense gap between screening and treatment. Postpartum women--particularly low-income mothers and mothers of color--obtain treatment for postpartum mood and anxiety disorders at abysmally low rates, even after they've been positively screened. Why?
There's also a little fact in the original research about the oxytocin receptor that's interesting. The study found that there was no connection between the oxytocin receptor and risk for PPD in women who had depression during pregnancy - the link was only in women who were not depressed prenatally. Not only does depression in pregnancy increase the risk for postpartum depression, but untreated prenatal depression is also a risk factor for unfavorable pregnancy outcomes including low-birth weights and pre-term births. So, we still need to screen all pregnant women AND treat those who are depressed. Other tidbits
The Massachusetts legislature overturned the Governor's veto of funding for the pilot program I mentioned above. I've been asking many of you in Massachusetts to contact your legislators about this recently, so thank you for all your advocacy!
Meanwhile, Congresswoman Katherine Clark and Congressman Ryan Costello introduced legislation, the Bringing Postpartum Depression Out of the Shadows Act, to increase and improve screening AND treatment for women with postpartum depression through grants to the states to develop new programs.
What's caught your eye in the news lately related to pregnancy or postpartum emotional complications?
|
Therapy, Groups, Supervision, Consultation, Training in Seattle, WA and online in Washington state
Laurie Ganberg, LICSW, PMH-C (#LW60673320) ~ Specializing in Perinatal Mental Health, Trauma, & Fat Liberation
Now practicing through Fiddlehead Therapy, PLLC with online services and in person in Mountlake Terrace, WA
Home | Privacy | Contact | Zoom Link
© 2019-2024 All rights reserved
Laurie Ganberg, LICSW, PMH-C (#LW60673320) ~ Specializing in Perinatal Mental Health, Trauma, & Fat Liberation
Now practicing through Fiddlehead Therapy, PLLC with online services and in person in Mountlake Terrace, WA
Home | Privacy | Contact | Zoom Link
© 2019-2024 All rights reserved