|
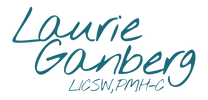
You've heard of PPD or postpartum depression. But what about perinatal emotional complications? Check out the infographic to learn 5 surprising facts about perinatal emotional complications. Sources are listed below.
Update: I've had some requests for hardcopies of this infographic, so I created a free PDF you can download.
[click infographic to enlarge]
Sources
Bornstein, D. (2014, October 16). Treating Depression Before It Becomes Postpartum. The New York Times. Retrieved from http://opinionator.blogs.nytimes.com/2014/10/16/treating-depression-before-it-becomes-postpartum/?_r=1
Dennis, C. L., & Chung‐Lee, L. (2006). Postpartum depression help‐seeking barriers and maternal treatment preferences: A qualitative systematic review. Birth, 33(4), 323-331. DOI: 10.1111/j.1523-536X.2006.00130.x. Foli, K. J. (2009). Postadoption depression: What nurses should know. AJN The American Journal of Nursing, 109(7), 11. DOI: 10.1097/01.NAJ.0000357144.17002.d3. Goodman, Janice H., and Lynda Tyer-Viola. Detection, treatment, and referral of perinatal depression and anxiety by obstetrical providers. Journal of Women's Health 19.3 (2010): 477-490. DOI:10.1089/jwh.2008.1352. Hamm, N. (2014, November 25). High Rates of Depression Among African-American Women, Low Rates of Treatment. Retrieved from http://www.huffingtonpost.com/nia-hamm/depression-african-american-women_b_5836320.html Hobfoll, S. E., Ritter, C., Lavin, J., Hulsizer, M. R., & Cameron, R. P. (1995). Depression prevalence and incidence among inner-city pregnant and postpartum women. Journal of Consulting and Clinical Psychology, 63(3), 445. http://dx.doi.org/10.1037/0022-006X.63.3.445 Howell, E. A., Mora, P. A., Horowitz, C. R., & Leventhal, H. (2005). Racial and Ethnic Differences in Factors Associated With Early Postpartum Depressive Symptoms. Obstetrics and Gynecology, 105(6), 1442–1450. DOI:10.1097/01.AOG.0000164050.34126.37. Huang, H. L., Peng, L., Zheng, S., & Wang, L. S. (2014). Observation on therapeutic effects of acupuncture plus psychological intervention for postpartum depression. Journal of Acupuncture and Tuina Science, 12(6), 358-361. DOI:10.1007/s11726-014-0805-7. Kim, P., & Swain, J. E. (2007). Sad Dads: Paternal Postpartum Depression.Psychiatry (Edgmont), 4(2), 35–47. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2922346/ Kozhimannil, K. B., Trinacty, C. M., Busch, A. B., Huskamp, H. A., & Adams, A. S. (2011). Racial and Ethnic Disparities in Postpartum Depression Care Among Low-Income Women. Psychiatric Services (Washington, D.C.), 62(6), 619–625. doi:10.1176/appi.ps.62.6.619. Nonacs, R. (2015, February 26). Treating Depression During Pregnancy Prevents Postpartum Depression. Retrieved from http://womensmentalhealth.org/posts/treating-depression-pregnancy-prevents-postpartum-depression/ Ross, L. E., Steele, L., Goldfinger, C., Strike, C. (2007). Perinatal depressive symptomatology among lesbian and bisexual women. Archives of Women's Mental Health. 10,(2), 53-59. DOI: 10.1007/s00737-007-0168-x. Smith, M. V., Kruse, A., Weir, A., & Goldblum, J. (2013). Diaper need and its impact on child health. Pediatrics, 132(2), 253-259. DOI: 10.1542/peds.2013-0597. Wisner, K. L., Sit, D. K., McShea, M. C., Rizzo, D. M., Zoretich, R. A., Hughes, C. L., ... & Hanusa, B. H. (2013). Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA Psychiatry, 70(5), 490-498. DOI: 10.1001/jamapsychiatry.2013.87. 
Two interesting news items related to postpartum depression popped up this past week. The first is news that researchers have identified a link between an oxytocin receptor blood marker in some women which increased their likelihood of experiencing postpartum depression. What does this mean? Well, if there were a blood test to give pregnant women to identify which ones were more likely to experience postpartum depression, we could proactively identify those women, doctors and families could put supports into place for the postpartum period ahead of time.
The second story is about a change in recommendations from the US Preventive Services Task Force about screening adults for depression. Now, if you're like me, you might be asking yourself what the US Preventive Services Task Force (USPSTF) is and what they do. Turns out, The Task Force is convened by Congress and reviews current clinical research to "improve the health of all Americans by making evidence-based recommendations about clinical preventive services such as screenings, counseling services, and preventive medications." This Task Force is now recommending that all adults be screened for depression because of its prevalence (1 in 10 all adults in the US will experience depression), and they specifically identified that all pregnant and postpartum women be screened. My reactions
It's great when postpartum depression gets media attention. It increases awareness of the huge number of families affected by emotional complications in pregnancy and postpartum . Screening and identifying those who are suffering is a critical first step.
However, there's an immense gap between screening and treatment. Postpartum women--particularly low-income mothers and mothers of color--obtain treatment for postpartum mood and anxiety disorders at abysmally low rates, even after they've been positively screened. Why?
There's also a little fact in the original research about the oxytocin receptor that's interesting. The study found that there was no connection between the oxytocin receptor and risk for PPD in women who had depression during pregnancy - the link was only in women who were not depressed prenatally. Not only does depression in pregnancy increase the risk for postpartum depression, but untreated prenatal depression is also a risk factor for unfavorable pregnancy outcomes including low-birth weights and pre-term births. So, we still need to screen all pregnant women AND treat those who are depressed. Other tidbits
The Massachusetts legislature overturned the Governor's veto of funding for the pilot program I mentioned above. I've been asking many of you in Massachusetts to contact your legislators about this recently, so thank you for all your advocacy!
Meanwhile, Congresswoman Katherine Clark and Congressman Ryan Costello introduced legislation, the Bringing Postpartum Depression Out of the Shadows Act, to increase and improve screening AND treatment for women with postpartum depression through grants to the states to develop new programs.
What's caught your eye in the news lately related to pregnancy or postpartum emotional complications?
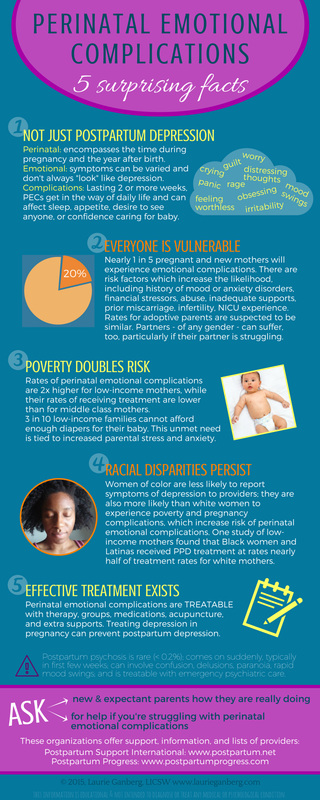
 Depression and anxiety are incredibly common both during pregnancy and after childbirth, but sometimes it's hard to get past the jargon and austere clinical descriptions of symptoms. Postpartum Progress features clear, accessible writing from real women who've experienced perinatal emotional complications - Warrior Moms - as well as professionals from all over the country. They also have a private forum and are hosting their first conference in Boston this summer! One of my favorite posts featured photos of women to demonstrate what it looks like when someone is suffering from a perinatal emotional complication (hint: not what you think!). "Plain Mama English" posts describing symptoms of postpartum depression, anxiety and psychosis are probably my other most referenced posts. You can even download nice PDFs to print out. Their newest tool is a New Mom Checklist for Maternal Mental Health Help, a checklist that a postpartum woman can bring to her care provider to start a conversation about getting help. This year is their third putting on the Climb Out of the Darkness, an awareness and fundraising event for Postpartum Progress and perinatal emotional complications. On June 20, there will be a Climb at Walden Pond in Concord, MA and others around the country where women who've experienced perinatal emotional complications and the people who support them will get together outside, create community, and symbolize the journey out of postpartum depression and anxiety and into the light of hope and recovery on the longest day of the year. You can find a climb near you or donate to my "couch" climb effort here. Postpartum Progress started exploring the needs of women of color who suffer perinatal emotional complications and surveyed women of color about their experiences at the beginning of 2015. I hope Postpartum Progress continues engaging and amplifying the voices of women of color, as well as exploring and increasing awareness of unmet needs of mothers of color. This post is part of the RESOURCES series where I feature websites, organizations, and information about perinatal emotional complications, parenting, therapy, reproductive health, and more. If you have a suggestion for a resource you'd like to see profiled, please let me know in the comments!  The PPD Awareness Day organized by the Massachusetts Legislature's Special Commission on Postpartum Depression, entitled Bringing Postpartum Depression Into the Light: Decreasing Stigma, Supporting Families, and Implementing Policy Change in Massachusetts, has been postponed due to the latest snow. As soon as it gets rescheduled, I'll share the news here.
There are some great speakers lined up including Dr. Gold, a pediatrician; Jamie Zahlaway Belsito, a postpartum depression survivor; Dr. Byatt, the Medical Director of MCPAP for Moms; Liz Friedman of MotherWoman; and Divya Kumar, a driving force behind a pilot project that put a postpartum doula in a community health center to provide accessible care, screening for perinatal emotional complications, and connection to clinicians for mothers there for their own or their children's medical appointments.
I'm hopeful that it will be an energizing afternoon where legislators can better understand the resources available - and not available - across the state, where mothers and families can meet with their representatives and providers there, and where more connections among us all can be made. I'll be there most of the afternoon at the PSI of MA table. Please come by and say hello! |
Therapy, Groups, Supervision, Consultation, Training in Seattle, WA and online in Washington state
Laurie Ganberg, LICSW, PMH-C (#LW60673320) ~ Specializing in Perinatal Mental Health, Trauma, & Fat Liberation
Now practicing through Fiddlehead Therapy, PLLC with online services and in person in Mountlake Terrace, WA
Home | Privacy | Contact | Zoom Link
© 2019-2024 All rights reserved
Laurie Ganberg, LICSW, PMH-C (#LW60673320) ~ Specializing in Perinatal Mental Health, Trauma, & Fat Liberation
Now practicing through Fiddlehead Therapy, PLLC with online services and in person in Mountlake Terrace, WA
Home | Privacy | Contact | Zoom Link
© 2019-2024 All rights reserved