|
I've moved upstairs in my building to suite 317B! The new office has a waiting room and is tucked away in a quiet corner in the back of the building. Most excitedly, it's large enough to run groups. There are still some final touches to make, but I'm seeing clients in this office as of July 1. I'll be offering the space for sublet for Monday day & evening and possibly one other evening. If you know any other therapists, nutritionists, coaches, or other folks who do group work, individual or family therapy, or consultations looking to start a practice or expand to a great Cambridge location, please put them in touch with me!  Senator Lovely speaking about her involvement with the PPD Commission. Senator Lovely speaking about her involvement with the PPD Commission.
I went to the screening of the maternal mental health documentary, Dark Side of the Full Moon, last night, organized by Leslie McKeough, LICSW - a Lynnfield therapist - and the North Shore Postpartum Depression Task Force. The documentary highlights the experiences of several women who experienced perinatal mood and anxiety disorders, the dismal state of screening for emotional complications in pregnancy and postpartum, and the barriers to treatment for these women. Interspersed are the news stories of the lives lost to maternal mental illness while they were filming the documentary.
Women feel guilty, self-conscious, isolated, and overwhelmed when they're experiencing emotional complications in the postpartum. Supporting women with perinatal emotional complications is about more than a 10-item questionnaire, though that's a good first step. It's about more than having a therapist's phone number, though that's needed too, and hopefully many people have that therapist's number or know where to look. It's knowing that if they reveal to you how they feel, they're doing so with fear and worry about not being a good mother, about their baby being "taken away," about never feeling like themselves again.
Supporting women with perinatal emotional complications is about having effective systems of care in the community that would include
These issues, this stigma, these barriers to care are why I and three colleagues founded the Every Mother Project with the belief that every mother deserves comprehensive perinatal support. We developed a Perinatal Toolkit for women's health professionals to better understand, recognize, know how to talk about, and support women through perinatal emotional complications. We've had lactation counselors, doulas, pelvic floor physical therapists, midwives, acupuncturists and many other birth and postpartum professionals download the toolkit. Our hope is that with more training and awareness for all the myriad of people who come into contact - and often develop quite close and important relationships - with pregnant and postpartum women and new parents, more women will feel heard and understood and will be able to be connected to the right supports. The movie didn't get into the racial and socioeconomic disparities that exist in maternal mental health, but I'd be remiss in not mentioning them here. There's been yet another study that examined stress in pregnancy and risk of postpartum depression, finding that more stress events (financial, partner, trauma, or emotional) in a woman's life was directly correlated with a higher risk for emotion complications. Other studies have identified that experiences of racial discrimination during pregnancy (which can be prevalent within medical systems) not only affect the pregnant woman's own emotional and physical health, but also impact the infant's stress physiology response. So yes, institutional racism and systemic oppression have real effects on pregnant and postpartum women of color and women in poverty, increasing their risk for perinatal emotional complications, all while making it harder for them to be identified and access treatment.
I'm so thankful for the chance to view Dark Side of the Full Moon, and that so many others did, too. We have much to do still to better support women through perinatal emotional complications - even in Massachusetts. Please, at least take a look at the trailer if you missed it. And maybe we can organize another viewing...
 Depression and anxiety are incredibly common both during pregnancy and after childbirth, but sometimes it's hard to get past the jargon and austere clinical descriptions of symptoms. Postpartum Progress features clear, accessible writing from real women who've experienced perinatal emotional complications - Warrior Moms - as well as professionals from all over the country. They also have a private forum and are hosting their first conference in Boston this summer! One of my favorite posts featured photos of women to demonstrate what it looks like when someone is suffering from a perinatal emotional complication (hint: not what you think!). "Plain Mama English" posts describing symptoms of postpartum depression, anxiety and psychosis are probably my other most referenced posts. You can even download nice PDFs to print out. Their newest tool is a New Mom Checklist for Maternal Mental Health Help, a checklist that a postpartum woman can bring to her care provider to start a conversation about getting help. This year is their third putting on the Climb Out of the Darkness, an awareness and fundraising event for Postpartum Progress and perinatal emotional complications. On June 20, there will be a Climb at Walden Pond in Concord, MA and others around the country where women who've experienced perinatal emotional complications and the people who support them will get together outside, create community, and symbolize the journey out of postpartum depression and anxiety and into the light of hope and recovery on the longest day of the year. You can find a climb near you or donate to my "couch" climb effort here. Postpartum Progress started exploring the needs of women of color who suffer perinatal emotional complications and surveyed women of color about their experiences at the beginning of 2015. I hope Postpartum Progress continues engaging and amplifying the voices of women of color, as well as exploring and increasing awareness of unmet needs of mothers of color. This post is part of the RESOURCES series where I feature websites, organizations, and information about perinatal emotional complications, parenting, therapy, reproductive health, and more. If you have a suggestion for a resource you'd like to see profiled, please let me know in the comments!
I've professed my love for Momma Zen: Walking the Crooked Path of Motherhood by Karen Maezen Miller before. I worry about parenting books that say "this -- my way -- is the way!" and their effect on vulnerable new moms looking for answers in the utterly chaotic early parenting days, but Momma Zen is different. Karen Maezen Miller says "I don't know either!" and compares the exhaustion of motherhood to a humidifier. Plus, the chapters are short: 3-4 pages and perfect for a quiet couple of minutes before bed, in the car while baby is sleeping, or while you're bouncing baby on a yoga ball.
This is the book I recommend and give to my friends who become mothers. And, just because, I'm giving away 2 autographed copies. Subscribe to my email newsletter to enter!
I've been getting lots of great responses in my survey of groups and classes for pregnant women, parents-to-be, and new parents. Please, keep them coming! If you're expecting a child, have a young child, or work with expectant and new families, please share your thoughts in the survey below. Responses are anonymous, but if you have any feedback or groups you want to share with me directly, please feel free to contact me! And if you want to be sure to get the compiled results and hear about next steps to meet the needs in the community, sign up for my newsletter.
 My dear friend and colleague, Divya Kumar, does amazing work. She's certified as a postpartum doula and lactation counselor, runs groups for new moms, and uses her public health background to develop and advocate for effective programs that actually improve access to comprehensive support for pregnant and postpartum women. All in the name of not just treating postpartum depression, but fostering emotional wellness. Here's my interview with her about the pilot program that was funded* by the state of Massachusetts to integrate postpartum support into existing medical systems. Tell me how the pilot program came about. DK: I was transitioning back to working outside the home after my second child was born and I started working as a postpartum doula. I have a public health background, and I tend to think in terms of systems and programs. I think about who has access to what services--and how and why. Every new mom can benefit from a postpartum doula, but not every mom knows what one is or can afford one, so I started thinking about how to increase access to postpartum doula services for all moms, and I thought it would be fantastic to have a postpartum doula in every pediatrician's office so that new moms could get emotional support, ask questions about things like sleep and soothing, and get help with breastfeeding. When my first child was a newborn, I had met Jessie Colbert at a local new moms' group. She is the administrative aide for Rep. Ellen Story, who chairs the Postpartum Depression Commission. So later, when I came up with the idea of integrating postpartum support into pediatric health settings, Jessie suggested that we develop this program as a postpartum depression prevention initiative. Rep. Story pushed for funding and the pilot program received $200,000 in 2013 to be split across four community health centers that serve a diverse patient population, including folks who are disenfranchised and under-served. What exactly does the pilot program look like? DK: The pilot looks a little different at the different community health centers, meaning that the centers have incorporated and built upon different aspects of perinatal care based on the capabilities of their own sites and the needs of their patients. In Lynn, mental health providers do home visits for new moms experiencing perinatal emotional complications. In Worcester, a team of OB advocates work with moms from pregnancy through the first two years of their child's life. In Jamaica Plain, we provide lactation support in our pediatric service, regardless of whether a baby's mom is a patient at the health center. What makes this different than other efforts to address postpartum depression?  DK: One of the big differences is that the pilot program integrates perinatal support into existing medical systems, and this integration reduces barriers and increases timely access to care for folks who need it. Being a new parent can be exhausting and overwhelming, and for folks who are disenfranchised by poverty or other extenuating circumstances, timely access to comprehensive services is key. At Southern JP Health Center (where I work), we see all new babies at their first pediatric visit--as early as 3 days postpartum! I come into the exam room after a physician sees a baby and screen the new mom for postpartum depression with the EPDS [Edinburgh Postnatal Depression Scale]. Also, providing comprehensive services means that we approach the mom and baby as a dyad. So, if a mom is struggling with perinatal emotional complications, I can connect her with a mental health provider in-house or in the community, and I can also help with issues within the dyad (breastfeeding and lack of sleep are the usual culprits here!) that can be exacerbating these complications. What difference do you see yourself and the program having in people’s lives? DK: I have had many moms tell me that they would have given up on breastfeeding if I hadn't walked into that exam room! It is such an honor to be in a position to help someone in that moment of distress. I have also walked patients who were having a mental or emotional health crisis up to our mental health department, where they were seen within the hour. Without screening them at their child's appointment, there's no way to know whether that crisis would have been identified and if they would have received mental health support. Also, I have had numerous moms contact me months after their babies were born to ask questions, get referrals, or just additional support, and many of these moms say to me, "It's so helpful to know that you're here to help me figure all of this out!" Having someone that they know they can contact with questions or concerns (especially those that are not directly related to their baby's health) is very reassuring for moms. What do you see happening next for the pilot program?
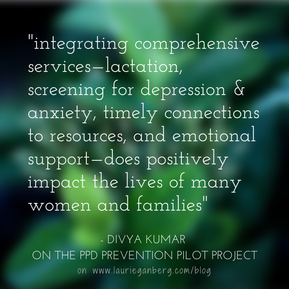
What’s one thing you would tell all mothers of newborns? DK: You're not supposed to do this by yourself! New moms are really isolated these days--many of us don't live with our parents or siblings, or in a home where friends and relative are constantly coming and going. I have heard many moms say, "I feel like I'm supposed to be able to do this by myself, but it's really hard!" Taking care of a newborn, figuring out breastfeeding, and adjusting to life as a parent involves a HUGE learning curve...while being utterly exhausted and recovering from the actual birth. Doing it yourself is often a very, very difficult task, and not one that new moms should have to take on. Ask for help. Accept help. Call a lactation professional. Call a friend. Go to a moms' group. Parenthood is better when we do it together! And, if I could tell expectant parents one thing, it would be to make a postpartum plan and get to know their local resources *before* their baby arrives. Make a list of lactation professionals, postpartum doulas, new parents' groups, meal delivery options, etc. I want to thank Divya Kumar for answering these questions and most importantly for all her work supporting new moms and advocating for better systems to care for new families. Have any questions for Divya? Continue the conversation in the comments! *In 2014, the funding for this pilot program was cut out of the budget. Rep. Story has again introduced a line item to fund the 4 locations of the pilot program in the new budget. Please consider calling your legislator to ask them to support budget line item 4510-0112. 03/06/2015 UPDATE: I'm excited to share that Kathleen Biebel, PhD, Program Director for MCPAP for Moms (M4M) was kind enough to add some comments and clarifications to my post. I'm including her words below in red. And, they are working on creating their own infographic, which will aim to capture some more of the subtleties of the flow of what happens when a woman and her medical provider contact MCPAP for Moms. Once it's available, I'll be sure to link to it.  Another unique-to-Massachusetts resource, MCPAP for Moms offers medical providers a Monday-Friday 9-5 phone line to speak to a care coordinator who can connect the provider to a MCPAP for Moms perinatal psychiatrist for consultation and/or help with connecting a mother and family to a community perinatal mental health provider. What does this look like? If a woman is at her OB's office or is talking to her primary care provider (PCP), and she feels comfortable sharing that she is struggling with anxiety or depression or other emotional complications in the postpartum period, her doctor can call MCPAP for Moms. The medical provider will get a call back from a MCPAP for Moms psychiatrist to discuss diagnostic questions or get guidance about a medication prescription. (They can (and do) discuss a whole range of issues that can also include depression screening, community mental health resources – it can really run the gamut). A MCPAP for Moms care coordinator can also provide referrals for therapists and support groups in the woman's community who specialize in postpartum mood and anxiety disorders. Since finding psychiatrists that have openings, who feel comfortable managing medication in pregnancy or while breastfeeding, and who accept insurance can be an enormous challenge, there is the great potential for this to help with more rapid connection to treatment for moms. (Absolutely! Another huge part of what M4M docs do is to help the calling provider start and/or continue to provide mental health care for perinatal women when appropriate. This is a huge goal of M4M – to support OB and PCP and psychiatric providers as they attend to the mental health care of their patients, and to increase their capacity and comfort in doing so). My concern about the program, however, is whether it will be effective in increasing access treatment for women of color, who frequently experience discrimination in the medical system. I wonder whether women of color will be willing to bring their questions about emotional health to medical providers, especially if those providers have not already screened for emotional distress. I look forward to hearing more from MCPAP for Moms about who they're reaching. (We at M4M share your concern that minority and under-resourced women are more likely to experience perinatal mental health concerns, and are less likely to access and engage in treatment. M4M aims to increase access to treatment for all women by increasing the capacity of providers serving perinatal women with mental health concerns. Our M4M docs, when working with calling providers, encourage depression screening, discuss a wide range of treatment options and considerations, review community based resources, etc. Our M4M docs work with providers with the information they share with us about their patients, which may or may not address someone's racial or cultural identity. We at M4M do not provide any direct treatment for women). Medical providers who are looking for more information about MCPAP for Moms can look here. I've talked with many folks who are unsure how the MCPAP for Moms process works, so I created a little infographic to help explain it. The information was gathered at meetings I have been at with MCPAP for Moms and their website and represents my understanding of the program. I'm not affiliated with MCPAP for Moms. This post is part of the RESOURCES series where every week I feature websites, organizations, and information about perinatal emotional complications, parenting, therapy, reproductive health, and more. If you have a suggestion for a resource you'd like to see profiled, please let me know in the comments!  Recently, there was a blog post by a new mother about how amazing her experience of motherhood was: "They should’ve warned me that my life was about to become so rich and beautiful and fulfilling, that I’d look back on what it was before and think, “Poor me. I didn’t know her yet.”". Predictably, there were responses decrying the one dimensionality of her piece: "I'm biased, having found the experience of parenting wonderful AND hard." This media hubbub about what we should be telling pregnant women and expectant couples about the realities of parenthood illustrates the conundrum of educating parents. Everyone's experience of the early postpartum period is different, influenced by their own health; their support system; their baby's temperament; their family of origin and history; their socioeconomic and work situation; their cultural, racial, and ethnic background; and countless other factors. I've been mulling all this over with my Becoming Parents Workshops. How do I offer a workshop to prepare parents-to-be to face common challenges inherent in life with a new baby, without resorting to scare tactics, all while acknowledging that neither I - nor they - can know what their reality will be until they're actually living it? Stumbling blocks are common issues that can arise for new parents. Some new mothers will be able to gracefully step over one or all of them. Others will be tripped up momentarily. And a few will be brought to their knees. But, recognizing these stumbling blocks makes it easier to avoid falling over them & to stitch together a safety net for the family. Balancing Needs 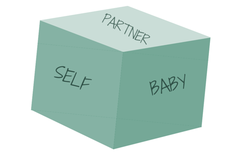 A newborn is completely dependent on her parents for nourishment, comfort, care, even for help burping. Of course meeting her needs is the priority; yet, I'm going to employ the tired airplane oxygen mask metaphor and say that mothers need to take care of their own needs in order to be able to take the best care of their babies. And where does the partner figure into this scenario? He or she also needs to figure out how to take care of their own needs. Then, both partners can be mindful of taking care of each other and their relationship. When parents feel like they're functioning well as a team, they're better able to handle the challenges of meeting baby's needs. The challenge is finding time and energy, and understanding the other's experience. It's a process to learn how to do this - I can't give anyone a magic formula (though I would if I could!) - but when a family goes through this learning curve to balance everyone's needs, they'll also be better able to shift how needs are met over time as the baby grows and the challenges change. Practical suggestions: Hire a postpartum doula for extra help in the early months, make sure each partner has opportunities to take care of the baby solo to gain confidence and competence and let the other partner get out of the house, put the baby down in a safe place when he won't stop crying and take 5 minutes with headphones on, or in the shower, or out on the porch to breathe and regroup. Reconciling Reality and Expectations 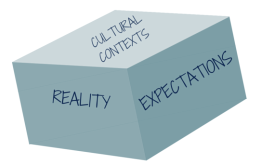 Imagining life with the baby is one of the joys of pregnancy. But it's inevitable that there will be discrepancies between those dreams and reality. Understanding how often a newborn baby needs to eat (8 to 12 times in a 24 period) and why (because their stomachs are tiny - only the size of an egg by weeks 2-3!) can help parents-to-be realistically anticipate life with baby. I spend time in my workshops talking about breastfeeding basics so that both parents can be on the same page and I make sure parents know where to turn for help if they run into challenges feeding the baby. Plans about, wishes for, and the reality of maternity/paternity leave also often clash. In the US, there's a propensity to think about maternity leave as "vacation" and I often see new mothers trying to do too much while they should be healing, learning and bonding with their baby, and taking care of themselves. And thanks to our lack of paid family leave, partners are often lucky if they can take 1 week off, while most mothers that I work with cobble together 6-12 weeks using sick time, vacation, short-term disability, and unpaid time off. There are other families that realize after the baby is born that the cost/benefit analysis of daycare and work shakes out differently and plans they made during the pregnancy change. Practical suggestions: Pregnant women can usually attend breastfeeding groups; if you're planning on breastfeeding I recommend going once before you have the baby. You'll likely see women nursing their babies; hear about breastfeeding realities, pumping, and a few tips/tricks; and meet the leaders or facilitators of the group. A friend pointed out that she was much more likely to contact one of the counselors at a local breastfeeding group once she'd met them, rather than cold-calling with a problem in the early days of her baby's life. Again, a postpartum doula can help new parents understand typical newborn behavior, develop and bolster trust in those parental instincts, and be a resource for questions about your baby. Babies are constantly developing and changing. When you think you have it figured out, your baby's going to switch it up; and when you think you won't be able to handle your baby's challenging behavior anymore, your baby's going to switch it up. Remind yourself "this will change" (without any pressure to enjoy it!). The same applies to new parents: make plans as best you can, but anticipate that you and those plans might change. Hint: there's usually not just one "right" decision. The who/what/why/how of asking for help 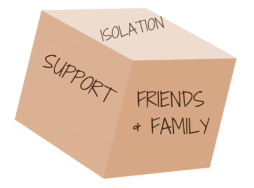 The last stumbling block I want to talk about is the tension between wanting time to adjust to being a new family of ___, understanding extended family's desires to meet the baby, making sure no one becomes isolated, and asking for help. Of course these building blocks are all connected and, often, expectations and reality need to be reconciled about how family or friends will help once the new baby arrives. Challenges frequently arise in relationships with parents and in-laws - now "the grandparents." Becoming a parent can be a time to reflect about your own childhood and identify ways you want to emulate your parents or do things differently. You may be surprised by your own strong opinions about how family members act with the baby and may be uncomfortable expressing your wishes. Or you may find that others can't follow through with what you ask of them and disappointment or anger rises. When family relationships are complicated, they often become more complex with the changes in family roles. For expectant couples who have lost parents, grief can resurface during pregnancy, birth, and the postpartum. A note about isolation: It is very easy to become isolated in the postpartum period. There are many cultures that prescribe a period of time (often 30-40 days) that a new mom stays at home with the baby, but often in these cultures, they are being visited by extended family and community members who are helping, talking with them, and taking care of them and the home. In the US, we have neither the cultural expectation that a new mother stay at home for a period of time, nor do we have the systems of support (visiting nurses, close family, family leave) that other countries and cultures create for new families. So parents-to-be are often left to build community around their new family, utilizing paid help when possible, friends/family/neighbors when available, and local formal and informal groups of other new parents. Practical suggestions: Spend some time during the pregnancy preparing a postpartum plan. We do this in my Becoming Parents Workshop. At a minimum, include specific information about local breastfeeding and new parent groups along with a plan for help with meals. Ask a friend or family member to set up a meal train (there are many, free options). On the baby registry, ask for an Instacart membership or other grocery delivery service. Once again, a postpartum doula can be a valuable additional support for those families that can afford to hire one - another thing to think about including on a registry if it's outside your means. Lastly, be aware of the signs of postpartum emotional distress and how the baby blues differ. If you find yourself or your partner struggling, please reach out for help. Postpartum Support International has an English and Spanish warmline available, or contact me. 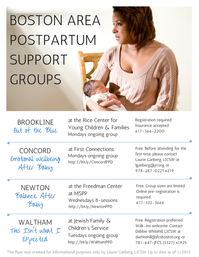 I've written before about why I think support groups are helpful. This resource is an informational flyer about four of the postpartum support groups in the Boston area. There are other groups that are run periodically by individual providers and other groups further afield. I find that with my practice in Cambridge and the work I do in Concord, these are the ones that I'm continually referring to, so I thought I'd make an easy flyer to share. I hope that lactation consultants, doulas, other therapists, OBs, midwives, childbirth educators and any one else that works with pregnant or postpartum women might share it with their clients so that if a new mom needs a group for support in the postpartum period with postpartum depression, anxiety, or general adjustment stress and challenges, they'll know where to turn!
 The PPD Awareness Day organized by the Massachusetts Legislature's Special Commission on Postpartum Depression, entitled Bringing Postpartum Depression Into the Light: Decreasing Stigma, Supporting Families, and Implementing Policy Change in Massachusetts, has been postponed due to the latest snow. As soon as it gets rescheduled, I'll share the news here.  I've been doing some volunteering for Postpartum Support International of MA so I'm especially eager to share that we have been updating the provider and support group listings available on the PSI of MA website or by calling their warmline at 1-866-472-1897. What's a warmline you ask? You call and leave a message and within 24 hours, a volunteer will get back to you to answer questions about postpartum depression, anxiety, and other adjustment challenges, as well as help connect you to providers and support groups in your area. If you're troubled what you or a family/friend is experiencing in the postpartum period and don't know where to start, the PSI of MA warmline is a great place to turn to talk to a knowledgeable, supportive trained volunteer. This post is part of the RESOURCES series where every Thursday I feature websites, organizations, and information about perinatal emotional complications, parenting, therapy, reproductive health, and more. If you have a suggestion for a resource you'd like to see profiled, please let me know in the comments!  In Boston, we're lucky enough to have the Center for Women's Health at Massachusetts General Hospital. Not only do they conduct and disseminate information about the latest perinatal research, but they offer consultations for pregnant and postpartum women. They recently had a look back of important posts on the blog from 2014, including their excellent response to the NY Times article on SSRI use during pregnancy. This post is part of the RESOURCES series where every Thursday I feature websites, organizations, and information about perinatal emotional complications, parenting, therapy, reproductive health, and more. If you have a suggestion for a resource you'd like to see profiled, please let me know in the comments! How did you come to start offering and be involved with the Expectant Mamas' Group? LS: When I really started seeing a lot of pregnant women in my practice, they were consistently telling me that they did not have any pregnant friends and were hoping to develop a community of people going through pregnancy at the same time they were. I initially started the group with a childbirth educator who wanted to start it as a paid program, but we had trouble getting it off the ground. She decided to stop working on it, but instead of shutting it down, I decided to keep it going as a free weekly discussion. It took some time to gain momentum, but since Erica joined it has become much better, more consistent, and with a wider variety of topics covered. EK: With my move to Boston in February 2013, I immediately became involved in the birthing community as a birth doula and photographer. I met Lizzie at the Partners in Perinatal Health Conference a few months after my move. She told me about the group and after coming to one meeting as a guest speaker I was hooked! It is such a fabulous resource and offers a safe place for new moms to meet other women, learn, ask questions, and be inspired.  I'm so excited to feature a two-for-one interview with Dr. Lizzie Sobel and Erica Kershner, the leaders of the Boston & Cambridge Expectant Mamas' Group. I hope you already know about this fabulous, free resource for pregnant women in the Cambridge area, but if not, head over to their Meetup page to learn about the group and upcoming speakers. Full disclosure: I'll be visiting on February 16th to talk about how couples can prepare for the postpartum period based on my Becoming Parents workshop. What could a newly pregnant woman expect if she went to a group? LS: We pick a different topic each week; sometimes Erica and I talk about a specific subject, sometimes we show a film about pregnancy or birth, and sometimes we invite special guests to speak with a wide range of expertise, such as home birth midwifery, breastfeeding, meditation, and more. No matter what the topic, a woman can expect to meet other pregnant women in the area, have a space to learn about pregnancy and birth, and also have lots of opportunities to ask questions and get answers. EK: We love keeping it as a casual discussion and we try to leave plenty of time for questions at the end. You can find the topics for each week posted on the meetup website. The Breathing Room, where we meet, is a warm and intimate space. It offers a great setting for our group. On a weekly basis we get anywhere from 3-15 guests which can include partners, friends and family. What happens after a woman gives birth? Do you ever hear from her again? LS: We love getting updates from our mamas about how their birth went. Many women tell us that they have made lasting connections with others in the group and consistently get together with them and their babies after they deliver. This is what our group is all about: helping women educate and empower themselves, and connecting them with a like-minded community of people going though the same big transition into Motherhood. EK: We love to hear from women after they give birth! It is always such a joy to hear the news from women who have shared and found value in the space. We have had many of the mamas come in as guest speakers to share their birth stories with the group and we want them to know they are always welcome back. What other resources or supports do you wish were available for pregnant or postpartum women in the Boston/Cambridge area? LS: I hear a lot of stress and anxiety about women going back to work and trying to balance their careers with their children. It would be awesome to see some kind of mentorship program where a pregnant woman could be connected with a working mom in her industry, to ask her questions about childcare, work/life balance, and just to have an emotional support person who understands what she is going through. [An aside from Laurie: I think this is such a great idea!] EK: Our group is unique in that it is geared toward pregnant women. There are many new moms groups offered around the Cambridge area but often the pregnancy groups are harder to find. Many of the women who come to the group are first time moms who are either new to the area, or don't have many friends who have children themselves. They are looking to meet other women that they can talk with and relate to. It would be a wonderful thing if there was more education around prenatal physical and mental wellness. Lizzie, tell us about being a chiropractor who treats pregnant women... LS: The most common complaints that bring a pregnant woman into my office are: low back pain, pubic symphysis pain, and round ligament pain. I also see a ton of women coming because their baby is not in an ideal position for birth: presenting breech, transverse, or occiput posterior. Chiropractic care can help with virtually any pregnancy related or non-pregnancy related ache and pain, ranging from migraine headaches, to wrist pain, to knee pain, to hip pain. I have also helped women who have urinary incontinence, constipation, and acid reflux, though this is not usually why they are presenting to the office. I have always wanted to help women have safer, easier, and more natural births. I believe very strongly that birth is a natural process, and that every woman has the innate intelligence to give birth without the use of drugs or surgery. After graduating chiropractic college, I started a year long postgraduate program in Westwood, MA through the International Chiropractic Pediatric Association. We met for an entire weekend each month for a whole year and learned all about treating pregnant women and infants and children of all ages. We learned practical adjusting, and also all the theory and information behind treating these populations. This training gave me the knowledge and confidence to start working with these unique populations. I immediately connected with the amazing birth community of Boston, and am able to help fill the great need for these services. I work very differently than many chiropractors. My adjustments are extremely gentle, with no cracking, twisting or popping. Most people feel extremely relaxed and even fall asleep during the treatments! If you are scared of going to a chiropractor, give me a call! I can guarantee that the adjustments will be comfortable and not at all scary. Erica, tell us about being a birth doula & photographer... EK: Dr. John Kennell once said "If a doula were a drug it would be unethical not to use it". Whether or not you are planning a natural childbirth, there are numerous benefits to hiring a doula. One of the biggest benefits is choosing an experienced birth worker that you know and trust who will be with you on your labor day. When birthing at a hospital, you most likely will have strangers coming in and out of your room throughout labor and birth. The doula (that you chose) will be with you from active labor until after the birth. She is working for you and no one else and is there to help you do all that is possible to get what you want out of the birth experience. She will be 24/7 support- there to guide and answer your questions- as you get closer to your estimated due date. I started doing birth photography soon after I began working as a doula. I studied photography at Mason Gross School of the Arts. It started by offering my doula clients photos and I was soon after being hired just for the photography portion. A few months later I found myself doing pregnancy, newborn and family sessions as well! There is so much beauty, love, and emotion surrounding birth. As a lifestyle photographer my favorite moments to capture are the raw emotion that happen in such intimate spaces and times. There is nothing more fulfilling than hearing from a client how much they treasure and are moved by the images. I want to thank Dr. Lizzie Sobel of Wholesome Healing Chiropractic and Erica Kershner of Birth Your Roots for answering my questions, and most importantly, for offering such a great resource to the community with the Expectant Mamas Group. Have any follow up questions? Post them in the comments and we'll see if we can answer them!
There are some great speakers lined up including Dr. Gold, a pediatrician; Jamie Zahlaway Belsito, a postpartum depression survivor; Dr. Byatt, the Medical Director of MCPAP for Moms; Liz Friedman of MotherWoman; and Divya Kumar, a driving force behind a pilot project that put a postpartum doula in a community health center to provide accessible care, screening for perinatal emotional complications, and connection to clinicians for mothers there for their own or their children's medical appointments.
I'm hopeful that it will be an energizing afternoon where legislators can better understand the resources available - and not available - across the state, where mothers and families can meet with their representatives and providers there, and where more connections among us all can be made. I'll be there most of the afternoon at the PSI of MA table. Please come by and say hello!  Becoming Parents workshops are scheduled for the first three months of 2015 for families welcoming a baby - by birth, surrogacy, or adoption - in the first half of next year. Sundays: January 11, February 8, or March 15 from 2-4pm in Somerville. While I am incredibly supportive of single parents, this workshop focuses on a couple's relationship, the realities of the effect of a newborn on the family, and how parents can support each other to be able to best take care of their baby. I welcome LGBTQ couples. Read more about the workshop and register here: Becoming Parents. |
Therapy, Groups, Supervision, Consultation, Training in Seattle, WA and online in Washington state
Laurie Ganberg, LICSW, PMH-C (#LW60673320) ~ Specializing in Perinatal Mental Health, Trauma, & Fat Liberation
Now practicing through Fiddlehead Therapy, PLLC with online services and in person in Mountlake Terrace, WA
Home | Privacy | Contact | Zoom Link
© 2019-2024 All rights reserved
Laurie Ganberg, LICSW, PMH-C (#LW60673320) ~ Specializing in Perinatal Mental Health, Trauma, & Fat Liberation
Now practicing through Fiddlehead Therapy, PLLC with online services and in person in Mountlake Terrace, WA
Home | Privacy | Contact | Zoom Link
© 2019-2024 All rights reserved